
There were two separate shellfish-associated outbreaks of illness in humans during the summer of 2012. One was in New York and the other Pontevedra, northwest Spain. The illnesses reported in Spain were believed to be one of the largest ever Vibrio outbreaks in this region.
These outbreaks were caused by people eating raw shellfish, which contained a marine bacterium called Vibrio parahaemolyticus. Previously this particular Vibrio strain had only appeared in the Pacific Northwest (PNW) region of North America.
Movement from PNW to the eastern seaboard of the USA and then across to Spain was unexpected and unprecedented. We want to find out how this strain moved over 6,000 miles from the Pacific to Europe.

Why should we care about such a tiny marine organism?
Some vibrios are capable of causing gastroenteritis - diarrhoea and vomiting in humans – and eating raw shellfish is the primary way we become infected.
These infections are rare in Europe. But these 2012 outbreaks suggest these bacteria could spread globally; this would be a significant public health issue.
The implications of the long-distance movement of the PNW vibrio strains are currently unknown. However, in the mid-1990s a new variant of V. parahaemolyticus emerged in Asia and quickly moved around the world, causing huge numbers of infections. The potential for this to happen with PNW strains must be recognised and assessed.
Also these bacteria grow in warm water. So we are concerned about how climate change may play a part in increasing clinical risk in Europe, as there have been several recent outbreaks related to warm-weather episodes.
Tell me more about vibrios and these particular strains.
Vibrios have a long history of causing disease in animals and humans. The most important Vibrio, from a human health perspective, is V. cholerae, which is responsible for cholera. Cholera spread throughout Europe and then to North America in the nineteenth century, and seven cholera pandemics have occurred in the past 200 years.
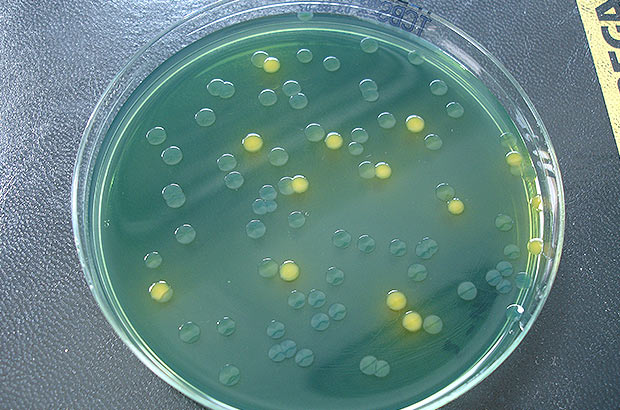
Vibrios are bacteria which look like curved, rod-like commas. They grow fast, are amazingly adaptable organisms and prefer to grow in warm low salinity water. Outbreaks tend to often follow warm-weather episodes. For example there were V. parahaemolyticus outbreaks during heat waves in the Northwest USA in 1997 and 2004.
But the PNW vibrio strains are particularly virulent at much lower doses when compared to other variants. These strains are genetically and biochemically distinct: they have a unique “finger print”.
Pathogenic strains normally carry one of two virulent genes and very rarely carry both. These genes can cause gastroenteritis. The PNW strains contained various combinations of both of these genes – something never seen before in Europe.
How do you know the PNW strains were the same as those found elsewhere?
Scientists from Cefas, the European Centre for Disease Prevention and Control (ECDC) and its American counterpart (CDC), and the USA’s Food and Drug Administration (FDA) collected samples which were then tested.
These tests included a range of “sub-typing” techniques used to distinguish strains. These tests are commonly used to track and pinpoint the strains responsible for outbreaks. Each test analysed and compared strains against a reference library of bacteria, which identifies specific vibrios based on similarities with other typed strains.
The results showed the strains from the Spanish and USA outbreaks matched to those from the PNW region. Again, this was the first time this strain had ever been found in Europe.
How did these strains move around, or were they always there?
We’re not certain how these strains crossed America and the Atlantic Ocean. But both the New York and Spanish outbreak sites are near deep-water ports. Ballast water in maritime vessels, the international trade and movement of shellfish produce and the long-distance ocean currents (e.g. the movement of the Gulf Stream) are all possible factors responsible.
Our scientists are currently analysing water, shellfish and plankton samples to build up an understanding of the mechanisms of possible transport.
Whether these strains persisted in the environment is also an important issue, so Cefas is analysing samples from across Europe. Their spread will have significant impact in terms of shellfish safety if they have the ability to survive during winter and reassert themselves when seawater temperatures rise.
What next? Can the scientists predict or prevent outbreaks in the future?
Monitoring bacteria in shellfish-production areas and other likely sites, even in cold weather, could help to identify any potential changes. But it is very early to be talking about predictive modelling.
Near real-time methods, such as satellite observations of coastal regions during heat waves, may help identify regions where these bacteria could emerge and pose a risk to the public. Such approaches are currently being developed by scientists at Cefas and ECDC.
Where can I go to find out more about how to eat shellfish safely?
There is useful information from the Food Standards Agency, Public Health England, National Health Service, and Seafood Health Facts
You can follow us on twitter @CefasGovUK.